Having a serious illness is often accompanied by physical pain. Living with this pain can make simple tasks hard to do- such as eating, sleeping, and basic household chores. Many people experiencing this pain often lose hope that their pain can be properly managed.
Pain is often difficult to control because it affects everyone differently. One person may have a higher “pain tolerance” as opposed to another. It’s always important to communicate your pain level with your doctor and/or nurse, as well as your caregiver. This will help in the future if you are unable to clearly say how much pain you are experiencing.
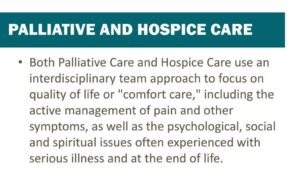
Enter hospice care! A team of experts who knows how to recognize the non-verbal and verbal pain signs, communicate among your hospice care team, and manages the patient’s pain so they can live the best quality of life! Freedom from pain and suffering is every patient’s right. Your pain can be managed. You do not need to suffer in silence or alone. St. Anthony’s Hospice cares for you and your pain.
Treatment Options
Chronic and serious pain are often treated with prescription medications. St. Anthony’s Hospice will take all factors into consideration (allergies, wishes, etc.) when creating the patient’s care plan.
Type: We choose the type of medication(s) based on the kind and level of pain, and how the pain affects the patient’s daily life. If one medication does not work well, we can try another or a combination. The pain medicine can be given by pill, liquid, injection, IV (at the Lucy Smith King Care Center), suppository, or patch.
Dose: Just like how people have different pain level tolerances, each person reacts differently to different doses of pain medication. The initial dose is based on the patient’s weight, height, age, level of pain, and medicines already being used. After the initial pain dose, the dosage can be adjusted to appropriately manage the patient’s pain level.
Schedule: Longer-acting medications can be taken on a schedule to treat pain over a length of time. “Breakthrough” or fast-acting medications can be taken as needed. Think of these fast-acting medicines as you taking an ibuprofen or acetaminophen for a headache.
There are several non-medication options you can use for pain. These include heat, ice, massage, stretches, or some light exercises. Other treatments that can help the mental side of pain include meditation, pet therapy, music therapy, aromatherapy, spiritual care, etc.

What can I do to keep my pain managed?
Always take your pain medication as prescribed. Even if you begin feeling better, don’t skip a dose! The goal of pain management is to be ahead of the pain, not fall behind and have to continuously catch up. Waiting for the pain to begin, may make it harder to manage.
Contact your St. Anthony’s Hospice nurse prior to taking other medications. This includes over-the-counter medicines, vitamins, or supplements.
Avoid alcohol when taking pain medication.
Appropriately store your medications. Keep medications in a locked drawer and away from children, pets, and others. Properly dispose of medications. You can ask your nurse for a medication disposal kit!
Keep notes to track your pain management plan and symptoms. Be sure to include when you take each dose, which medication and dose you take, side effects, location and type of your pain, rate pain before medication and 60 minutes after dosage.
Talk to your nurse! If your pain medicine either isn’t working or if you are experiencing odd mental side-effects, let your nurse know so they can work with your provider to change your medication.
Hospice Myth
Two common myths come around when talking about hospice care and pain management. “Hospice care takes away all your medications” and “hospice care just gives you morphine, so you are out of it the whole time.”
Hospice takes away all medications. Hospice care is all about managing pain and symptoms, which the most common way is with medications. This does not mean that hospice providers over-medicate their patients or remove all medications. While many patients are over medicated prior to coming into hospice care, and your hospice physician and nurse will look at your prescription medication list and remove some medications, we do not remove them all. This “de-prescribing” is used to reduce medicines that have heavy side effects of ones that are not benefitting the patient, thus decreasing their quality of life. We dove deeper into this myth in a previous blog post that you can find here.
Hospice care just gives your morphine, so you remain out of it or unconscious the whole time. While morphine is a commonly used hospice pain management medication, it is not over-used. When morphine and other pain management medications are used as prescribed and for medical reasons, patients will have the much-needed relief without the “out of it” or “loopy” feelings.
If your or a loved one has been diagnosed with a serious illness and you are needing extra care, please call St. Anthony’s Hospice or Palliative Care at (270) 826-2326. You can also make an online referral here.