Living with a life-limiting illness is never what you have in mind for yourself or a loved one. What if you are told that a cure is no longer attainable? Where do you go from there? Where do you want to be?
When the possibility of a cure is gone, hope is not. Through hospice care, there is still hope for no pain or suffering; hope for a peaceful death; hope to be at home for your final months, weeks, days, hours, and minutes; and hope to be surrounded by loved ones and pets.
“While there isn’t one specific point in an illness when a person should ask about hospice care, many hospice professionals would suggest that a person think about hospice long before he or she is in a medical crisis,” advises J. Donald Schumacher, president and CEO of the National Hospice and Palliative Care Organization. “In fact, learning about palliative care and hospice as options is something that should happen early in the course of a serious illness and not just in the final days.”
Hospice is not a place. Hospice is provided wherever the patient calls home- house, apartment, nursing home, assisted living facility, or our hospice inpatient unit, the Lucy Smith King Care Center. Hospice care involves an interdisciplinary team of clinicians and trained volunteers to ensure all of the patient’s needs are being met and all types of pain are being treated- physical, psychological, social, financial, and spiritual. Each patient has his/her own care plan tailored to his/her individual needs.
Hospice care not only helps patient maintain their dignity and independence as well as increase quality of life, it also helps the family as well.
“Hospice professionals can be important resources for patients and families, they can help a person figure out what goals are important and help them get their arms around the fact that their life may be coming to a close,” noted Schumacher.
Hospice care is considered to be the ideal model for the most compassionate, highest quality care for those nearing the end of life. It offers the services and support that most Americans want when facing a life-limiting illness.
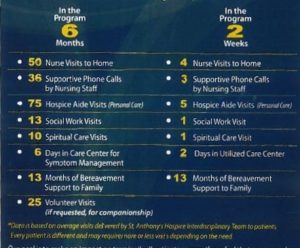
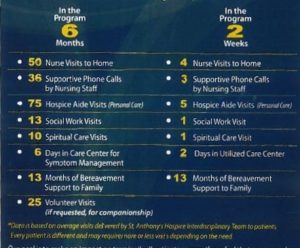
Nearing the end of life does not necessarily mean the patient is close to death. While hospice care is for patients with a life-limiting illness that should the illness run it’s normal course, the patient has a life expectancy of 6 months or less However, when a patient’s physical, psychological, spiritual, financial, and social symptoms are properly managed, a patient can live for much longer. If hospice care is started early in the disease process, a patient receives more benefits!
According to the NHPCO 2020 facts and figures data, in 2018 1.55 million Medicare beneficiaries received hospice care, which is a 4% increase from 2017 (1.49 million beneficiaries). Also according to the NHPCO in 2018, 1.1 million Medicare beneficiaries died while enrolled in hospice care. Over half of the deaths occurred in the patient’s home and more than 1/3 was split between nursing homes, hospice inpatient facilities, and assisted living facilities.
Facts about hospice care
- The majority of hospice care is provided in the patient’s home. Hospice care is also provided in skilled nursing facilities, assisted living facilities, and hospice inpatient units.
- Hospice care is 100% covered by Medicare, Medicaid, and some private insurances. Anthony’s Hospice will not turn anyone away based on inability to pay.
- It is a common myth that hospice care only treats cancer patients. However, hospice care treats anyone diagnosed with any life-limiting illness. These life-limiting illnesses can include, but are not limited to, various cancers, COPD or other respiratory illnesses, CHF or other heart illnesses, COVID-19, sepsis, kidney illnesses, Alzheimer’s Disease, ALS, MS, many neurological conditions, cirrhosis or other liver diseases, and AIDS.
- Not only does hospice include the interdisciplinary team, it includes durable medical equipment, medical supplies, and medications related to the patient’s hospice diagnosis.
- While a physician does not have to make the hospice referral, one does have to certify that the patient is seriously ill and the patient has a life expectancy of 6 months or less, should the disease run its normal course. This does not mean that the patient will die in 6 months or less.
- Hospice also offers bereavement services for the patient’s family. St. Anthony’s Hospice offers grief support for 15 months after the loss of their loved one. Bereavement services are offered to anyone, regardless if they had a loved one pass with St. Anthony’s or not.
“Ideally, an individual would receive hospice care for the final months of life – not just the final days,” stated Schumacher. “One of the most common sentiments from families who have been helped by hospice care is that they wish they had known about hospice or been referred to hospice sooner.”
Hospice care is available 24/7! While the patient’s care team won’t be in the home with him/her all day, every day; a hospice nurse is available to a patient at any time of any day. If the patient had a fall at 2am, has trouble breathing at 7pm, or passes away at 5:30am, a nurse is one phone call away. The hospice nurse will come assist the patient and family. One of the main goals of hospice care is to keep the patient where he/she wants to be, and not in the hospital.
The longer a patient is with hospice care, the more benefits the patient receives. Hospice care does not mean you or a loved one is “giving up”. Hospice care is hope for the patient and family, as well as help.
If you or a loved one needs extra help managing a serious illness or has any questions, please call St. Anthony’s Hospice at (270) 826-2326.
Sources: file: https://www.nhpco.org/wp-content/uploads/NHPCO-Facts-Figures-2020-edition.pdf
https://www.prnewswire.com/news-releases/when-is-it-time-for-hospice-111451104.html