May we never forget the tragedy of 9/11/01. It’s been 19 years and we can still remember where we were and what we were doing when news broke of the first plane crash.
Where were you when the world stopped turning?
May we never forget the tragedy of 9/11/01. It’s been 19 years and we can still remember where we were and what we were doing when news broke of the first plane crash.
Where were you when the world stopped turning?
In an ideal world, family and loved ones would pass away quietly, in their sleep. They would be surrounded by loved ones and comfortable until the end. Sometimes with visitor restrictions or social distancing, we must tell loved ones “goodbye” over the phone or FaceTime.
This is the farthest thing from ideal. Many hospitals, nursing facilities, assisted living facilities, etc. try to accommodate family members who cannot be in the room when a loved one is imminent. Staff members will hold a phone up to the patient’s ear, use speakerphone, or turn on FaceTime to allow loved ones to say goodbye when they cannot be in the room.

How to Say Goodbye Over the Phone
Stay focused. Focus on your loved one and your relationship with him/her. Block out others in the room and talk specifically to your loved one.
Share the phone. If more people are needing to say goodbye, be sure everyone gets the amount of time they need. Allow others to have their moment.
“I love you” goes a long way. Three words pack a ton of meaning and emotion into them. Don’t hold back, say them as much as you want.
Thank them. It’s likely you’re on the phone because the person had a deep influence on your life. When you say thank you to them, you are letting them know how much of an influence they had on your life. Thank them for the love they have showed you or things they taught you.
Ask for forgiveness. Relationships are hard. We can hurt someone we love in large or small ways. Don’t dwell on the small things. However if something is weighing on you, be sure to apologize for it. Just keep in mind your loved one may respond positively, negatively, or not at all. Take ownership of your faults and know you did what you could to right the wrong(s).
Forgive. Your loved one may ask you for forgiveness for any pain they may have caused. They may not be able to speak due to advance in their state. Regardless of words or actions, you can tell your loved one that you forgive them and free yourself from carrying that burden for the rest of your life.
Relive memories. If you have time to move outside of the love, thankfulness, and forgiveness to relive some memories you two share. Talk about special holidays, trips you’ve taken together, favorite recipes, weddings, or outings you took together Laugh about inside jokes and particular memories. If you’re not alone on the phone, allow others to join in and share memories you all share together. It’s always important to surround your loved one with love and laughter, even in their final moments.
Last conversations are never easy, but they are something you take with you for the rest of your life. It’s always harder when you can’t be with your loved one in the end and you have to have your final conversation over the phone or FaceTime. Just reminding your loved one how much they mean to you, how loved they are, and that they will always be remembered in your heart goes the longest way.
If you or a loved one is in need of hospice, palliative, or bereavement care, please contact us at (270) 826-2326 to learn more.

Having your wishes heard and honored is always important, especially during a pandemic. Advance care planning is making decisions about the care you wish to receive, if you become unable to speak for yourself. These decisions are usually in writing and provided to family and your healthcare provider. The decisions you make about your care are put in an “Advanced Directive” which is a legal document that takes effect only if you become unable to communicate your wishes or speak for yourself. One could become unable to communicate healthcare wished due to serious injury or disease, regardless of one’s age. The legal documents help loved ones make decisions for you and help your healthcare provider know what type of medical care you wish to receive.
There are a few types of Advanced Directives one should have in place while healthy and of sound mind to make such important decisions. These documents include a Living Will and Healthcare (or Medical) Power of Attorney. A Living Will allows a person document his/her wishes regarding medical treatments at the end of life. A Healthcare (or Medical) Power of Attorney allows a person to appoint a surrogate or person he/she trusts to be the healthcare agent, who is authorized to make medical decisions on the person’s behalf.
Prior to your Living Will guiding your medical care, two physicians must certify that you are unable to make medical decisions, you are in the medical condition stated in the document (i.e.- terminal illness or incapacitated), or the state the document was prepared in/person’s residence could have other requirements.
Prior to your Healthcare (or Medical) Power of Attorney going into effect, your physician must certify you are unable to make decisions and if you regain the ability to make decisions, the surrogate cannot continue to make decisions and other requirements required by the state the document was prepared in/person’s residence.
St. Anthony’s Hospice has social workers who can assist patients and family with these documents. While our social workers are not attorneys, they do have the knowledge to make the legal documents easier for the average person to understand. They can also assist the family and patients with funeral arrangements, if they need help with that.
If we can help you or a loved one feel more comfortable or getting advanced directives in place, please call us at (270) 826-2326 or visit our website at https://stanthonyshospice.org/referral/.
“’Palliative care’ means patient and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering.” -definition from CMS webpage
What does “suffering” mean to you or a loved one facing a serious illness? Is it being in physical pain? Is it being lonely? Or is it something else?
What does quality of life mean to you or a loved one facing a serious illness? Increased comfort? Emotional happiness? Or something else?
Healthcare today treats illnesses and not a patient’s suffering. While we are grateful there are professionals who treat illnesses, perform surgeries, and cure diseases, we also want our suffering treated. There is not a person on this earth who has not felt suffering. When a baby is born, he/she comes out crying. Kids, teens, adults, and elders have also all experienced a form of suffering- whether emotional, physical, spiritual, or another form.
Palliative care is the part of healthcare and more specifically, hospice care, that is designed to manage the suffering a patient typically feels with his/her terminal diagnosis. Palliative care improves quality of life in all dimensions of the phrase. Palliative care is a huge part of hospice care.
Why do we overtreat in healthcare, to the point where hospice and palliative care are used in a patient’s final days to hours of life? If everyone agreed that quality of life is the most important thing, healthcare would be better than it already is.
We have not failed when a patient cannot be cured. If a person cannot be cured, it is time to heal the person. One can go into the healthcare system completely broken and come out fixed. This is always fantastic when it can happen! When you go into the healthcare system and cannot be fixed, hospice care and palliative care can heal you. Your body may be failing, but your quality of life and your dignity are healed.
If you or a loved one is needing extra help in treating suffering, please call St. Anthony’s Hospice at (270) 826-2326.
Living with a life-limiting illness is never what you have in mind for yourself or a loved one. What if you are told that a cure is no longer attainable? Where do you go from there? Where do you want to be?
When the possibility of a cure is gone, hope is not. Through hospice care, there is still hope for no pain or suffering; hope for a peaceful death; hope to be at home for your final months, weeks, days, hours, and minutes; and hope to be surrounded by loved ones and pets.
“While there isn’t one specific point in an illness when a person should ask about hospice care, many hospice professionals would suggest that a person think about hospice long before he or she is in a medical crisis,” advises J. Donald Schumacher, president and CEO of the National Hospice and Palliative Care Organization. “In fact, learning about palliative care and hospice as options is something that should happen early in the course of a serious illness and not just in the final days.”
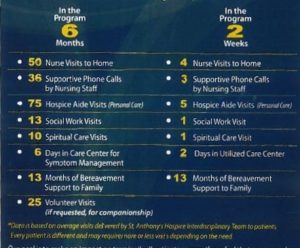
Hospice is not a place. Hospice is provided wherever the patient calls home- house, apartment, nursing home, assisted living facility, or our hospice inpatient unit, the Lucy Smith King Care Center. Hospice care involves an interdisciplinary team of clinicians and trained volunteers to ensure all of the patient’s needs are being met and all types of pain are being treated- physical, psychological, social, financial, and spiritual. Each patient has his/her own care plan tailored to his/her individual needs.
Hospice care not only helps patient maintain their dignity and independence as well as increase quality of life, it also helps the family as well.
“Hospice professionals can be important resources for patients and families, they can help a person figure out what goals are important and help them get their arms around the fact that their life may be coming to a close,” noted Schumacher.
Hospice care is considered to be the ideal model for the most compassionate, highest quality care for those nearing the end of life. It offers the services and support that most Americans want when facing a life-limiting illness.
Nearing the end of life does not necessarily mean the patient is close to death. While hospice care is for patients with a life-limiting illness that should the illness run it’s normal course, the patient has a life expectancy of 6 months or less However, when a patient’s physical, psychological, spiritual, financial, and social symptoms are properly managed, a patient can live for much longer. If hospice care is started early in the disease process, a patient receives more benefits!
According to the NHPCO 2020 facts and figures data, in 2018 1.55 million Medicare beneficiaries received hospice care, which is a 4% increase from 2017 (1.49 million beneficiaries). Also according to the NHPCO in 2018, 1.1 million Medicare beneficiaries died while enrolled in hospice care. Over half of the deaths occurred in the patient’s home and more than 1/3 was split between nursing homes, hospice inpatient facilities, and assisted living facilities.
Facts about hospice care
“Ideally, an individual would receive hospice care for the final months of life – not just the final days,” stated Schumacher. “One of the most common sentiments from families who have been helped by hospice care is that they wish they had known about hospice or been referred to hospice sooner.”
Hospice care is available 24/7! While the patient’s care team won’t be in the home with him/her all day, every day; a hospice nurse is available to a patient at any time of any day. If the patient had a fall at 2am, has trouble breathing at 7pm, or passes away at 5:30am, a nurse is one phone call away. The hospice nurse will come assist the patient and family. One of the main goals of hospice care is to keep the patient where he/she wants to be, and not in the hospital.
The longer a patient is with hospice care, the more benefits the patient receives. Hospice care does not mean you or a loved one is “giving up”. Hospice care is hope for the patient and family, as well as help.
If you or a loved one needs extra help managing a serious illness or has any questions, please call St. Anthony’s Hospice at (270) 826-2326.
Sources: file: https://www.nhpco.org/wp-content/uploads/NHPCO-Facts-Figures-2020-edition.pdf
https://www.prnewswire.com/news-releases/when-is-it-time-for-hospice-111451104.html
Our Business Development Coordinator, Riley Hamilton, made a couple of videos for a recent virtual health fair we participated in. We wanted to share her videos with all of you!
Hospice Care video- https://youtu.be/XOG1advPxao
Palliative Care video- https://youtu.be/Ov_I9Dw48Wg
If you have any questions, please call our office at (270) 826-2326.
Instead of the normal Why St. Anthony’s post, we wanted to talk a little bit about grief, especially with the pandemic still in full force.
Grieving is a natural part of life and at St. Anthony’s Hospice, we can help you along the way. St. Anthony’s offers monthly grief groups, child and adult grief counseling, grief support classes, and Although the COVID-19 pandemic has thrown a wrench in our monthly grief support groups, our Bereavement Coordinator is still assisting people in their own homes. Unfortunately, our wee, kids, and adult camps are all cancelled due to the pandemic, but we normally have bereavement camps during different times of the year.
If you or a loved one needs hospice or palliative care, or needs help coping with the loss of a loved one, please call our office at (270) 826-2326. One of the best things about hospice care is the care isn’t only for the patient, it helps the family/caregiver as well! St. Anthony’s bereavement support continues for 15 months after your loved one passes away. Just another few reasons “Why St. Anthony’s” provides the best end of life care for patients and families.
![Grief in Children [Infographic] | Crosswinds Counseling](https://i1.wp.com/crosswinds.org/wp-content/uploads/2016/10/Blog-Infographic-Grief-in-Children-e1571263976172-824x1024.jpg?resize=824%2C1024&ssl=1)
Source listed on image.
Hospice is…
Hospice is about quality of life, not death.
Hospice is about keeping your dignity, even after you’ve passed away.
Hospice is support and extra help when the patient and family need it.
Hospice is comfort in all definitions of the word for the patient.
Give us a call to see how we can help your loved one at (270) 826-2326!

We’re adding another installment of “Why St. Anthony’s” to our website! Taylor Vernam has kindly shared the story of her grandmother, Priscilla Vernam and her grandmother’s sister, Linda Abell; both who passed away with St. Anthony’s care.
“Why St. Anthony’s?” is unfortunately one of the easiest questions for our family to answer. I had always heard great things about St. Anthony’s Hospice and the Lucy Smith King Care Center but never thought I would experience it firsthand with loved ones… twice… in the same year. February 9, 2018 began our first of two experiences at the Lucy Smith King Care Center with my grandmother, Priscilla. After being diagnosed with cancer, only 9 days prior to being admitted, the next 9 days became the longest. My mom and I were told the worst news we had ever heard on February 18, at 3:52 a.m. “I’m sorry ladies, but she has passed.” Fast forwarding to July 2, Linda, my grandmother’s sister, became a patient in the care center after also being diagnosed with cancer. After being there in February and having a great experience with the staff, we as a family were at ease knowing that another family member was going to be well taken care of. At this point we knew the staff, the rooms, and the family room all too well; they even remembered all of us as we entered the unit. July 5 at 1:05 a.m., it became a nightmare that none of us could believe was happening again. Two nurses and two aide’s stood around us as we heard the terrible news again. I can distinctly remember everything about those two early mornings, but that isn’t the first thing that comes to mind when I speak of our loved ones’ time under the care of St. Anthony’s. What I think about is the heartfelt care and compassion that each staff member had for my grandmother, aunt, myself and our family. From the referral process to the memorial leaf hanging in the care center, every nurse, aide, volunteer, etc., has been nothing short of wonderful and concerned for our grieving. I truly cannot thank St. Anthony’s Hospice enough for what they have done for our family.”


We’re digging through our vault to bring back another edition of Why St. Anthony’s. Today’s post comes from August 9, 2019 and was submitted by our Lucy Smith King Care Center Administrative/Assistant/Unit Secretary, Amy Hanley.
“Caring for and loving people when they need it most has always been a part of who I am. My current position with St. Anthony’s Hospice presented itself to me in August 2017. Without hesitation, I immediately applied and prayed that this was where I was meant to be. I love to love people. I love to comfort others when there is a need. And this organization exemplifies just that and so much more. People often ask us “how do you do it everyday? How do you work around such sadness?” St. Anthony’s Hospice is about so much more than the sadness, sickness, death, and dying. To me, the answer is simple… I get to work in a place that is filled with so much compassion, selflessness, kindness, and love everyday. I leave my job everyday feeling so fulfilled, knowing that we have gone above and beyond to treat patients and their families with the same compassion and dignity that we would all want for our own loved ones and families, not because we have to, but because that’s who we are as people and an organization, and what we believe in and stand for. The best part of my job is doing what I love and loving what I do everyday. They say it’s a beautiful thing when a career and a passion come together, and I am so blessed and thankful that it has for me.”
