Have you ever paid attention to how your provider talks about treatments and how much like war-talk there is?
Really think about it…
“We’re going to win this battle with cancer.”
“Let’s rally behind Aunt Sally for her battle with breast cancer.”
“The infection has infiltrated his kidneys.”
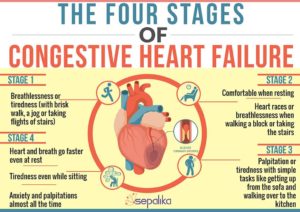
“She’s having a heart attack.”
Ultimately life is not a battle to be won; nobody comes out alive. But don’t think about it in a negative light. Life is a gift! A beautiful gift given to each and every one of us that allows us to make a difference. Using your senses to explore the world is a privilege.
For religious people, life does not just end at death. Some believe in reincarnation. Some believe in an eternal afterlife. Some believe we only continue to exist in memories. Regardless of the differences in beliefs, death is a mysterious part of life that nobody really knows what happens when that time comes.
How do you know when to switch from the “warfront” of traditional medicine to embracing what is to come and living out the remainder of your life with the best quality care?

Dying comes in stages- denial, anger, bargaining, depression, and acceptance. Not everyone experiences all 5 steps or even in that order. If one of these steps has been a person’s mindset their entire life, there is a bigger chance they will go out that way. For example, if a person has been angry their whole life, they may approach death feeling angry. Same goes for denial, depression, bargaining, and acceptance.
Whatever the person’s mood or however close they are to accepting their inevitable fate, we always face the question, “when do I stop aggressive treatment? when do I shift to hospice care?” Shifting from fighting for a longer life to a fuller life is never easy but hospice care is there to help.
Nearing the end of life does not necessarily mean the patient is close to death. While hospice care is for patients with a life-limiting illness that should the illness run it’s normal course, the patient has a life expectancy of 6 months or less. A patient must meet hospice eligibility requirements set by the Centers for Medicare and Medicaid Services. You can see a list of general eligibility requirements here.
We’ve said it so many times, hospice does not hasten death! Rather, when a patient’s physical, psychological, spiritual, financial, and social symptoms are properly managed, a patient can live for much longer. If hospice care is started early in the disease process, a patient receives more benefits!
Beginning hospice care early in the terminal diagnosis, ensure all symptoms are expertly managed which improves quality of life and can even improve quantity of life. The patient receives care from nurses, aides, social workers, and chaplains in the location of their choosing. Many patients receive care in their own home or in an assisted living facility, skilled nursing facility, or the Lucy Smith King Care Center. Hospice care is considered to be the ideal model for the most compassionate, highest quality care for those nearing the end of life. It offers the services and support that most Americans want when facing a life-limiting illness.
Hospice care uses an interdisciplinary team approach. This means we treat the whole person, from their physical symptoms to psychological to social to spiritual, and everything in between. Hospice care allows patients to keep their current physician, should their physician choose to follow, and their current caregiver! We don’t force loved ones to stop caring for the hospice patient, we encourage them to continue and empower them by teaching valuable skills and educating on the disease and dying processes.
“Human beings are physical, psychological, spiritual, and social entities and ought not to be reduced to any one dimension. The notion of totality of a holistic approach to the person is critical in all dimensions of health care.” -Ron Hamel, Making Health Care Decisions.
When initially diagnosed with a life-limiting illness, our focus should be completely on curing the patient and/or defeating the disease. At this point, the patient should consider a palliative care referral. Visit our website here to learn about the difference in hospice and palliative care.
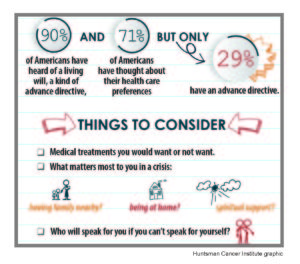
We should always have those “what ifs” in the back of our mind to be realistic.
“What if we get to a point where the treatments aren’t working?”
“What if my quality of life is really taking a hit with these treatments?”
Be prepared and pay attention to look for the signs that your quality of life is taking a hit. Check out an article on quality indicators for end of life care here. Or just think about it- can you tolerate more treatments without being sick or extremely weak? Do I feel up to doing things I have always loved like going out to eat, going on a walk, gardening, visiting with friends or family or pets, etc.?
Encourage your loved one to listen to that internal voice that says “I’m done” or “Enough is enough.” Once you hear that voice, it’s time to shift the focus from treating the disease to treating the person. Always remember, when you are told “there’s nothing more that can be done,” there is always more that can be done! Meaning it’s time to focus on quality of life!
A dying person is still a person. They can still hear, feel, love, cry, see, etc. They are just a person with a shorter life expectancy. Grant your loved one’s wishes. Go to the beach one last time. Take a boat ride. Go for a picnic in the park. Just sit and listen to stories about their life. Focus on increasing that quality of life! Even under St. Anthony’s Hospice care, we don’t limit you to being homebound. We help our patients honor their last wishes and travel. Now, that doesn’t mean we pay for it, but we do help find the help the patient needs. For example, if your loved one wants to go to Florida for vacation, we contact a hospice provider wherever you go in Florida to be sure the patient is still getting the quality care needed while traveling.
Hospice care is exceptional end of life care. It’s not admitting defeat or giving up. Hospice gives the patient the quality of life and dignity they so deserve.
If you know me personally, you know I’m a big Queen fan. I wanted to close this out with some lyrics from “Who Wants to Live Forever” that I think pertain really well to focusing on quality of life and not fearing death.
“Who wants to live forever
There’s no chance for us
It’s all decided for us
This world has only one sweet moment set aside for us
Who wants to live forever”
Our fate has already been decided for us. We aren’t promised another day, so many every day count.
If you or a loved one is in need of palliative or hospice care, please call us at (270) 826-2326 or make a referral here.
Sources for this blog post- https://www.bmj.com/content/bmj/291/6511/1820.full.pdf and
CareNotes “Hospice Care: When Enough is Enough” by Fr. Dick Sparks, C.S.P., Ph.D.