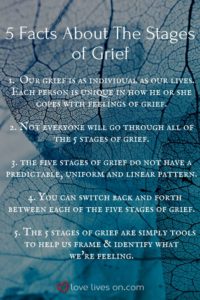
You may have heard that grief occurs in set stages: denial, anger, depression, ,bargaining, and acceptance. However, no two people grieve in the same way so how can we classify everyone into certain stages?
Instead of grief looking like this:

It often looks more like this:

Not everyone experiences all of the stages of grief, and some people may hit a stage farther down in the list and revert to one earlier in the list. These “stages of grief” are merely a tool to help us identify what we are feeling after experiencing a loss. These stages were developed by a Swiss-American Psychiatrist named Elisabeth Kübler-Ross. She wrote a fantastic book entitled On Death and Dying in 1969, where she discussed the 5 stages of grief. You can read more about her biography and pioneering grief studies by checking out this link. For now, we are going to dive into what each stage looks like.
Denial Stage
“This can’t be happening.”
“But I feel great! How can I have cancer?”
“I just saw Grandpa last week and he seemed fine. I can’t believe he died last night.”
It is completely normal to rationalize your overwhelming emotions. This is a common defense mechanism that helps absorb the blow of the immediate shock.
We tend to block out the truth and hide from the facts. This is a temporary response that carries us past the first wave of pain we experience after a loss. Once you explore the situation surrounding your loss, reality tends to set in. There’s no time limit on the denial stage. It’s your body’s way of protecting itself.
Be open to seeing reminders of your loved one, as painful as it may be. Visit the gravesite, look through old pictures, listen to their favorite songs, or wrap yourself in your loved one’s favorite clothing or blanket. Talk through your denial with family, friends, or a grief counselor.
Anger Stage
“This is all your fault!”
“It’s Nana’s fault she got lung cancer. She smoked 10 packs/day for 65 years! Now she’s gone and I have to deal with all of this pain.”
“Dr. So-N-So didn’t do anything at all to cure Aunt Susie’s COPD! It’s his fault she died!”
In the “anger stage” we tend to search for someone to blame, feel intense guilt ourselves, and lash out at loved ones or even the decedent. As the numbing effects of the denial stage wear off, you may not be ready to cope with the loss of a loved one, so you express your intense pain as anger. Your anger doesn’t have to be logical or invalid. For example, you are mad at Dr. So-N-So for not curing Aunt Susie’s COPD when you know he did what he could but COPD can’t be cured.
Honor your anger! Allow yourself to be angry and express it! We don’t mean pick a fight with someone. Express your anger in a healthy manner- go for a run, try out a kickboxing class, find a solitary place and just scream. Don’t keep your anger all bottled up. Explore it in a way that doesn’t harm yourself or others. Talk through your anger with family, friends, or a grief counselor.
Bargaining Stage
“What if we went for a 2nd opinion? Would Grandma still be here?”
“What if I am nicer to everyone and start doing community service, God? Will you spare Uncle Jim’s life?”
This bargaining stage of grief may seem silly, but it serves an important purpose. It provides a temporary escape from the pain you are experiencing and provides hope. This temporary escape gives you time to adjust to the realness of the situation. Sometimes when attempting to bargain with God, feelings of guilt aren’t far away.
Talk to family, friends or a grief counselor about your bargaining hopes and wishes. They may be able to provide you with some perspective and help you through this phase.
Depression Stage
Intense sadness, decreased or increased sleep, reduced appetite, loss of motivation.
Depression usually occurs when reality officially sets in. This stage feels like it lasts forever, because our grief transitions into present-day and the depression hits on a level much deeper than anything experienced thus far in the grief stages. It’s important to know the depression experienced in the stages of grief is not a sign of mental illness. However, if you are experiencing suicidal thoughts or actions, please seek immediate professional help!
Give yourself time to feel your emotions. Don’t let anyone tell you to “get over it” or simply “move on”. In order to healthily heal, you must acknowledge your pain. Avoiding your depression associated with grief can transition into chronic depression, anxiety, substance abuse, or other mental/physical illness. Talk to family, friends, or a grief counselor to express your feelings. You can even do something creative to express these feelings; write a letter to your loved one, create a photo album or scrapbook of your loved one, create a playlist of your loved one’s favorite music or music that reminds you of him/her, or volunteer at a place your loved one thought was special or a place that took care of your loved one.
Acceptance Stage
“I’ll never be okay with losing my grandma, but I cannot let my grief control my life.”
Acceptance does not mean you are “okay” with the loss of your loved one. Most people don’t ever feel “okay” about losing someone they love. The acceptance stage is still a process, it isn’t a final stage with an ending.
Understand that the acceptance is learning to live with the new normal in your life, not that you must be “okay” with the loss. Be patient with yourself. It may take some people years to reach this stage, while others may reach it quickly and bounce back to denial several times before fully accepting the new norm. Talk to family, friends, or a grief counselor to help reach the acceptance stage and come to terms with your new normal.
Unfortunately, grief and loss are some things everyone experiences at one point in his/her life. St. Anthony’s Hospice offers FREE grief support and counseling to anyone, not just families of hospice patients. We believe everyone should have a safe and healthy way to manage their grief. Please call us at (270) 826-2326 or visit our bereavement page.
Sources of photos found on photos.










![Grief in Children [Infographic] | Crosswinds Counseling](https://i1.wp.com/crosswinds.org/wp-content/uploads/2016/10/Blog-Infographic-Grief-in-Children-e1571263976172-824x1024.jpg?resize=824%2C1024&ssl=1)