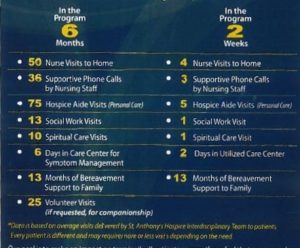
The month of September is Pain Management Awareness Month! It was first declared this in 2001 when the American Chronic Pain Association (ACPA) led a partnership of groups to establish such.
Pain management is one of the primary goals of hospice care- keeping patients comfortable and managing symptoms to ensure the highest quality of life for as long as they may live. Not all patients experience pain near the end of life but treating pain and other symptoms effectively is crucial. The hospice care team continues to evaluate the patient’s pain at every visit. They use pain rating scales as well as monitoring the nonverbal signs of pain.
How Pain is Determined
How many times have you been to the doctor or hospital where he/she asks you “on a scale of 1-10, what your pain level?” This is a common and universal communication tool in healthcare. It allows patients to rate their pain or point to one of the faces to help the clinician understand the patient’s pain level and better manage it. Below is an example of the commonly used/seen pain scale chart. The chart ranges from no pain whatsoever to the worst pain possible.
Image from Google image search- “pain scale”
If there is a nonverbal patient, hospice clinicians can look at how a patient is acting to assess pain level. For example, a nonresponsive or sleeping patient may grimace, his/her chin may quiver, jaw may be clenched, he/she may be kicking their legs or tensing them up, he/she could squirm, moan or whimper or cry, or he/she could be difficult to comfort or be extremely distracted. St. Anthony’s Hospice wants all patients to be comfortable and have the highest quality of life in a patient’s final months, weeks, days, hours, and minutes.
Pain signs for Caregivers
When caring for a loved one who has been diagnosed with a serious illness, the caregiver must know what to look for. Here are some signs to look for:
- Increased breathing rate
- Tightly closed eyes or rapid blinking
- An increase in the patient’s systolic blood pressure from their baseline
- Holding arm or leg muscles tightly or a rigid body posture
- Rocking, fidgeting, or pacing
- Resisting care or guarding certain areas of the body when turning
- Becoming withdrawn
- Becoming more aggressive or easily angered
- Crying
- Increased confusion
- Vocalizations such as moaning, calling out, sighing, and asking for help.
Pain Management Misconceptions
One common misconception about hospice care is that hospice clinicians medicate the patient so much that he/she is constantly sleeping or “out of it.” While hospice care does involve medication to keep the patient comfortable, that’s just it. We want the patient to be comfortable and pain-free and still able to interact with loved ones, if the patient still can. Hospice care utilizes opioids to ensure the patient is pain-free. Hospice nurses educate the caregiver on how to administer the medication to the patient. All hospice patients and caregivers are informed of and sign our opioid medication protocol. Opioid addiction is not a concern at the end of life; often there is not enough time to develop an addiction in 6 months or less. Addiction for the patient should not be a concern, rather using the effective tools is more important. Controlled substances do not hasten death. Studies have proven the opposite! These medications do not prolong life however if a patient’s symptoms are properly managed, quality of life increases thus increasing quantity of life!
Emotional, Spiritual, and Social Pain
We’ve often said that hospice care treats all types of pain. But what does this mean? Physical pain is what we most often think of when we think of pain. Emotional, spiritual, and social types of pain are huge players in increasing quality of life. Emotional pain, like anxiety or depression, can increase a person’s physical pain and vice versa. Emotional pain is treated both with medications such as Ativan, and regular visits from the patient’s social worker and chaplain, who also works to treat the patient’s spiritual pain. Social pain is eased by interacting with people other than the primary caregiver. Social pain is especially important to treat during the COVID-19 pandemic. St. Anthony’s Hospice is taking precautions to ensure our patients and staff are staying negative.
Family members and caregivers should be careful to not add to the patient’s stress and anxiety by arguing with or in front of the patient.
What if I have a loved one who is experiencing a lot of pain?
If you or a loved one needs pain managed due to a serious illness, give St. Anthony’s a call- (270) 826-2326. Our clinicians work hard to ensure our patients have the best quality of life by controlling all types of pain.