The liver is an organ in the body that is essential for detoxing the blood, production of bile, certain proteins for blood plasma, cholesterol to help carry fats through the body, regulating blood clotting, and many others. It is the largest solid organ (2nd largest in the body, to the skin) and located in the right upper quadrant of the abdomen, under the ribcage.
Liver failure and liver disease are two different things. Liver disease refers to any condition that causes inflammation and/or damage to your liver. Liver disease affects the overall function of the liver. Liver failure is when your liver has lost some to all of its functionality. Liver failure often occurs from the damage caused by liver disease.
One amazing fact about this organ is that it can repair and even regenerate itself, if the damage is caught early enough! Many people with liver disease do not look or feel sick, even though their liver is becoming damaged. At a certain point, the liver damage becomes irreversible and can lead to liver failure, cancer, or death.

Common Causes of Liver Disease
- Viruses, such as Hepatitis A, B
- Genetics
- Certain autoimmune diseases
- Excessive alcohol consumption
- Poor diet/obesity
- Reactions or overuse of certain medications, street drugs, or other chemicals, such as acetaminophen, certain antibiotics, or certain herbal supplements
Symptoms of Acute Liver Failure
- Feeling unwell
- Fatigue
- Nausea or vomiting
- Abdominal pain and/or swelling
- Jaundice- yellowing of the skin and eyes
- Confusion or disorientation
Symptoms of Chronic Liver Failure
Early symptoms
- Fatigue
- Appetite loss
- Nausea or vomiting
- Abdominal discomfort and/or pain
Advanced symptoms
- Jaundice
- Easily bruised or bleeding
- Confusion or disorientation
- Edema, buildup of fluid in abdomen, arms, or legs
- Dark urine
- Severe skin itching
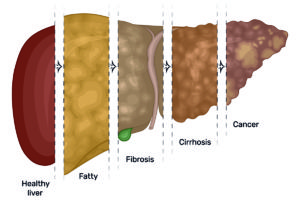
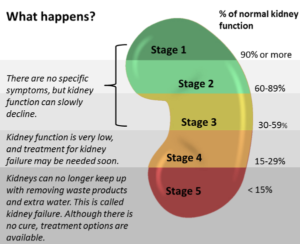
Stages of Liver Failure
Damage from liver failure can occur in several stages. Each stage increasingly affects the liver’s ability to function. Just like we previously said, “Liver failure is when your liver has lost some to all of its functionality. Liver failure often occurs from the damage caused by liver disease.”
Inflammation
In the early stages of liver failure, inflammation occurs. This means your liver becomes enlarged and/or inflamed (“a localized physical condition in which part of the body becomes reddened, swollen, hot, and often painful, especially as a reaction to injury or infection”). Many people with inflammation don’t experience symptoms. However, if the inflammation continues, permanent damage occurs. Inflammation can be hard to detect since there are usually no symptoms.
Fibrosis
If no treatment is sought when you are diagnosed with liver inflammation, the liver may begin to scar over. Excessive buildup of scar tissue on the liver is called liver fibrosis. If left untreated over time, the excess scar tissue replaces the healthy, normal liver tissue. As scar tissue replaces normal tissue, this greatly impacts the function of the liver. The buildup of scar tissue can even reduce or stop blood flow through the river. Fibrosis can be difficult to detect because of the lack of symptoms. If a patient with liver fibrosis seeks medical attention and treatment, there is a possibility the liver can heal.
Cirrhosis
Cirrhosis is a late-stage scarring of the liver. This late-stage fibrosis can be caused by excessive alcohol consumption or certain conditions/diseases. Many people begin to notice symptoms once cirrhosis has began. Without treatment, it can worsen and damage can be irreversible. As a result, the liver may stop properly working or may stop functioning at all. Treatment may be able to stop or delay liver damage, you cannot reverse damage caused by cirrhosis.
End-Stage Liver Disease
When a person reaches end-stage liver disease (ESLD), the liver’s function has deteriorated so much that the person requires a liver transplant. Some physicians may refer to this as chronic liver failure. With ESLD, some people may develop ascites (the accumulation of fluid in the abdominal cavity which causes abdominal swelling) and the development of ascites has an average life expectancy of 6 months or less , if it doesn’t respond to treatment.
Palliative and Hospice care can greatly benefit those with liver disease and/or failure. Both work to improve quality of life however with hospice care, the patient is no longer seeking curative treatment and/or a liver transplant. Call St. Anthony’s Hospice or Palliative Care at (270) 826-2326 or make an online referral to see how either program can benefit you or a loved one.
Sources found here, here, and here. Definitions linked on term above. Photo sources here and here.