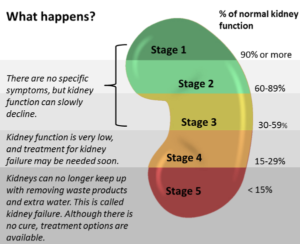
Chronic Kidney Disease (or CKD) refers to lasting kidney damage that progressively worsens over time and all 5 stages of kidney damage. These stages range from very mild (stage 1) to complete kidney failure (stage 5) The stages of CKD are based on the kidney’s ability to filter waste and extra fluid from the bloodstream. In the early stages, a person’s kidneys can still filter waste but in the later stages, your kidneys will have to work harder to get rid of waste or may not be able to do so at all. Over 30million people in the United States are living with CKD. How your physician measures your kidney function is by the estimated glomerular filtration rate (or eGFR). The eGFR is a number based on your creatinine levels, which is a waste product in your blood.
While anyone can be diagnosed with CKD, some risk factors that increase your risk include:
1. Diabetes
2. High Blood Pressure
3. Heart Disease
4. Family History of CKD
5. Being African American, Hispanic, Native American, or Asian
6. Being over 60 years old
Understanding the different stages of CKD can help a patient be more educated on the disease process and make appropriate healthcare decisions. We wanted to help you learn more about this disease.

Stage 1
In stage 1 CKD, you have mild kidney damage and an eGFR of 90 or greater. Most of the time, this means your kidneys are healthy and functioning well but you do have other signs of kidney damage. These signs of kidney damage can include protein in your urine or actual physical damage to your kidneys. Some ways to slow the progression of CKD if you are in stage 1 include:
– Controlling your blood sugar if you are diabetic
– Control your blood pressure
– Maintain a healthy diet
– Don’t smoke/vape or use smokeless tobacco
– Strive for 30 minutes of exercise at least 5 days per week
– Maintain a healthy weight
– Talk to your doctor about medications or vitamins to help protect your kidney function
– Get an appointment with a kidney doctor, or nephrologist, even though you have a primary care provider
Stage 2
In stage 2 CKD, you have mild kidney damage an eGFR between 60%-89%. Most of the time, this means your kidneys are healthy and functioning well but you do have other signs of kidney damage. These signs of kidney damage can include protein in your urine or actual physical damage to your kidneys.
Some ways to slow the progression of CKD if you are in stage 2 include:
– Controlling your blood sugar if you are diabetic
– Control your blood pressure
– Maintain a healthy diet
– Don’t smoke/vape or use smokeless tobacco
– Strive for 30 minutes of exercise at least 5 days per week
– Maintain a healthy weight
– Talk to your doctor about medications or vitamins to help protect your kidney function
– Get an appointment with a kidney doctor, or nephrologist, even though you have a primary care provider
Stage 3
Stage 3 is split into 2 stages, Stage 3a and Stage 3b. In Stage 3a, you have an eGFR between 45%-59%. In Stage 3b means you have an eGFR between 30%-44%. This means there is some damage to your kidneys and they are not functioning as well as they should be.
Many people do not exhibit symptoms in Stage 3, but if you are exhibiting symptoms they can be:
– Swelling in the hands and/or feet
– Back pain
– Urinating more or less than normal
Also in Stage 3, a person is more likely to start having health complications as waste builds up in your body. These can include:
– High blood pressure
– Anemia, or a low number of red blood cells
– Bone disease related to hyperphosphatemia or high levels of phosphorus in the blood
To prevent Stage 3 CKD from progressing, you can:
– Control your blood sugar if diabetic
– Control your blood pressure
– Don’t smoke/vape or use smokeless tobacco
– Eat a healthy diet and meet with a dietitian
– Exercise for at least 30 minutes, 5 days per week
– Get to and maintain a healthy weight
– Visit a nephrologist in addition to your primary care provider
– Ask your physician about medications to control your blood pressure and those to improve kidney function
Stage 4
Stage 4 CKD means you have an eGFR between 15%-29%. This means your kidneys are moderately to severely damaged and not working as well as they should. Stage 4 is the last stage before kidney failure and should be taken very seriously. Stage 4 is where palliative care can benefit the patient!
Many people begin to exhibit symptoms in Stage 4, which can include:
– Swelling in the hands and/or feet
– Back pain
– Urinating more or less than normal
Also in Stage 4, you will likely have health complications as waste builds up in your body. These can include:
– High blood pressure
– Anemia, or a low number of red blood cells
– Bone disease related to hyperphosphatemia or high levels of phosphorus in the blood
To prevent your Stage 4 CKD from progressing to complete kidney failure, you should:
– Regularly see your nephrologist
– Meet with a dietitian to help with your healthy diet
– Regularly take blood pressure medications as prescribed by your doctor
In Stage 4 it is time to begin talking with your nephrologist about the starting dialysis or preparing for a kidney transplant.
Stage 5
Stage 5 CKD means you have an eGFR less than 15%. This means your kidneys are either getting very close to failure or they have completely failed. If your kidneys fail, waste will build up in your blood which makes you very ill. Stage 5 is where hospice or palliative can help!
Some of the symptoms of kidney failure include:
– Itching
– Muscle Cramps
– Nausea & vomiting
– Not feeling hungry
– Swollen hands and feet
– Back pain
– Urinating more or less than normal
– Trouble breathing
– Insomnia (or trouble sleeping)
Once your kidneys have failed, kidney transplantation or dialysis are your treatment options. However, should you choose quality of life, hospice can help! If you choose quality of life in tandem with your treatment, palliative care can help! A kidney transplant is when a donor kidney is taken and transplanted into your body. If you can find a living donor, you may be able to plan for a kidney transplant and palliative care earlier. Dialysis assists your body in removing excess water and waste from the blood when your kidneys can no longer do it themselves. Palliative care can be used in conjunction with a kidney transplant and/or dialysis.

Palliative Care and Chronic Kidney Disease
When a patient is facing late-stage kidney disease (stage 4 or 5), St. Anthony’s Palliative Care team can help to manage symptoms and bridge the gap between the patient and their physician/nephrologist by providing an extra set of eyes and ears in the home. Palliative care can also help the patient access additional resources and support in the community.
Our palliative care team helps patients match their care plan to their personal goals as the patient explores options from transplant to dialysis to comfort care only.
To learn more about St. Anthony’s Hospice or Palliative Care, please call us at (270) 826-2326 or make a referral online.
Resources for this article found here.
